Abstract
Introduction
The prognosis of patients with myelodysplastic syndromes (MDS) depends on several disease characteristics such as the cytopenias, the percentage of bone marrow blasts, and the cytogenetic profile of the patients. The use of hypomethylating agents (HMAs) has altered the prognosis of patients with higher risk MDS offering a median survival of around 24 months. Nevertheless, the range of survival is wide, with some patients achieving long remissions and high survival rates irrespective of their initial prognostic characteristics. Long-term survivors after 5-azacytidine administration constitute a large group of patients with potentially special characteristics and needs.
Aim
We analyzed data from a large cohort of patients with MDS treated with 5-azacytidine to describe the hematologic and prognostic characteristics of long-term survivors and compare them to those of patients with shorter survival.
Patients and Methods
We retrospectively recorded through the Hellenic 5-azacytidine registry the main demographic, hematologic and treatment characteristics of adult patients with MDS treated with 5-azacytidine monotherapy. Patient data from 28 centers meeting the 2008/2016 WHO diagnostic criteria for MDS were recorded during a 7-month period.
We defined two groups of long-term survivors based on their survival after initiation of treatment with 5-azacytidine (OST). The first group comprised patients with OST above the third quartile (Q3 or 75th percentile) of the whole group (Q3 group) and the second patients with OST above the 90th percentile of the whole group (P90 group). Correlations were made between long- and short-term survivors for both groups.
IBM SPSS statistics, version 23.0 (IBM Corporation, North Castle, NY, USA) was used for the statistical analysis of the results.
Results
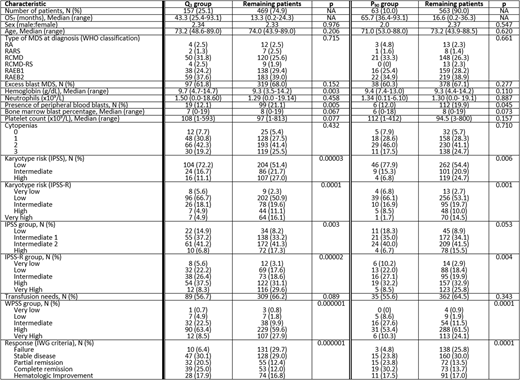
Data from 626 patients was recorded. The Q3 group comprised 157 patients with an OST longer than 24.5 months (median, 43.3 months) and the P90 group 63 patients with an OST longer than 36.4 months (median, 65.7 months). The detailed characteristics of the two groups along with comparisons with the remaining patients with OST below Q3 and P90 respectively are shown in Table 1. Data analysis revealed that the sex, the age, the type of MDS at diagnosis per the 2008/2016 WHO classification, the presence of excess (≥5%) marrow blasts, the number of cytopenias, the hemoglobin, neutrophil and platelet count, and the transfusion needs were not predictive of long-term survival in neither of the groups. On the other hand, the presence of peripheral blood blasts, the karyotype risk, the IPSS, IPSS-R and WPSS classification and response to treatment were predictive of long term survival in both groups (Table 1). Multivariate analysis revealed that response to 5-azacytidine was the strongest determinant of long-term survival (Kaplan Meier, Log Rank, p<0.0001) in a model comprising IPSS, IPSS-R, WPSS and response to treatment. Nevertheless, patients with stable disease were almost equally distributed in the groups of long- and short-term survivors (p=0.795 for the Q3 group and p=0.310 for the P90 group).
Discussion
The use of HMAs in MDS has increased survival rates, hence long-term survival is now a feasible target when managing such patients. One fourth of the patients of this registry achieved an OST over 24.5 months and 10% over 36.4 months. IPSS, IPSS-R and WPSS are powerful prognostic tools for patients with MDS. Among the prognostic components of IPSS and IPSS-R at diagnosis (cytopenias, bone marrow blast count, karyotype risk), the karyotype risk seems to be the stronger determinant of survival. Nevertheless, among long-term survivors there are patients with adverse prognostic characteristics at diagnosis, whose prognosis is altered by the administration of HMAs. Failure to respond to 5-azacytidine is a major determinant of OST, but stable disease was not correlated to survival in this cohort. This result highlights the importance of continuing treatment with hypomethylating agents in patients not achieving an optimal response (PR, CR, HI), since a significant proportion of them may achieve long survival rates. Further search for new clinical and/or molecular prognostic markers is warranted to identify the prognosis of patients with MDS and define those who would benefit from the use of HMAs or other upcoming treatment choices.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal